Hidradenitis Suppurativa Face: Effective Treatment Options
Hidradenitis suppurativa (HS) is a chronic skin condition characterized by recurrent, painful abscesses and nodules, typically occurring in areas with apocrine glands, such as the armpits, groin, and buttocks. However, in some cases, HS can also affect the face, leading to significant discomfort, emotional distress, and social stigma. Facial hidradenitis suppurativa can manifest as inflamed, pus-filled bumps, or nodules on the face, often accompanied by swelling, redness, and scarring.
Understanding the complexities of facial HS is crucial for effective management and treatment. While the condition shares similarities with other forms of HS, its location on the face requires specialized consideration due to the sensitive nature of facial skin and the potential for significant cosmetic and psychological impact.
Problem-Solution Framework: Identifying Challenges and Solutions for Facial HS
One of the primary challenges in managing facial HS is distinguishing it from other skin conditions, such as acne, rosacea, or folliculitis, which can present with similar symptoms. Accurate diagnosis by a dermatologist is essential, as it guides the treatment approach. Once diagnosed, patients often face a myriad of treatment options, ranging from topical and oral medications to surgical interventions, each with its benefits and drawbacks.
Topical Treatments
For mild cases of facial HS, topical treatments may be prescribed. These can include:
- Antibiotics: To reduce bacterial infection and inflammation.
- Retinoids: Derivatives of vitamin A, which can help prevent clogged pores and reduce inflammation.
- Corticosteroids: To decrease inflammation and prevent scarring.
Oral Medications
For more severe cases, oral medications might be necessary:
- Antibiotics: Systemic antibiotics can help control infection and reduce symptoms.
- Hormonal treatments: For women, especially if HS is linked to hormonal fluctuations.
- Retinoids: Oral retinoids, like isotretinoin, can be very effective but come with significant side effects and require close monitoring.
Biologics
Biologic medications, such as adalimumab, have shown promise in treating moderate to severe HS, including facial manifestations, by targeting specific components of the immune system.
Surgical Options
In advanced cases where significant scarring or persistent lesions are present, surgical interventions might be considered:
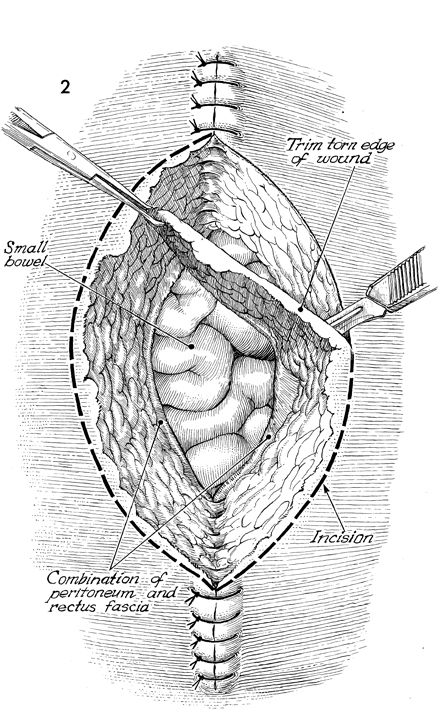
- Incision and drainage: For acute abscesses.
- Deroofing: A procedure that involves removing the roof of the tunnel under the skin.
- Excision: Removing the affected area entirely, which may require skin grafting.
Comparative Analysis: Evaluating Treatment Effectiveness
Each treatment option has its efficacy, risks, and benefits. Topical treatments are generally well-tolerated but may not be sufficient for severe cases. Oral antibiotics and hormonal treatments can be effective but may have side effects or not be suitable for long-term use. Biologics offer a promising approach with potentially fewer systemic side effects than traditional oral medications but are typically reserved for severe cases due to cost and potential immune system implications. Surgical options can provide relief for advanced disease but carry risks associated with any surgical procedure.
Expert Interview Style: Insights into Managing Facial HS
According to dermatological experts, managing facial hidradenitis suppurativa requires a multifaceted approach that considers not only the severity of the condition but also the patient’s overall health, lifestyle, and personal preferences. “It’s crucial to educate patients about the nature of their condition, the importance of adhering to treatment plans, and the potential need for lifestyle adjustments, such as weight management, smoking cessation, and stress reduction,” notes Dr. [Expert’s Name], a leading dermatologist specializing in HS.
Decision Framework: Choosing the Right Treatment
When deciding on a treatment plan, several factors must be considered:
- Severity of Symptoms: More severe cases may require oral medications or biologics.
- Previous Treatments: What has been tried before and with what success?
- Patient Preferences: Some patients may prefer topical treatments to avoid systemic side effects.
- Potential Side Effects: Weighing the benefits against potential risks.
- Lifestyle Considerations: Travel, work, or personal commitments that may impact treatment adherence.
Future Trends Projection: Emerging Therapies for Facial HS
The landscape of hidradenitis suppurativa treatment is evolving, with ongoing research into new biologic agents and other therapeutic modalities. Advances in understanding the pathophysiology of HS, including its association with the immune system and potential links to the microbiome, are expected to yield more targeted and effective treatments. Furthermore, there is growing interest in the role of diet, stress management, and other lifestyle factors in managing the condition, potentially offering patients more holistic approaches to care.
Conclusion
Facial hidradenitis suppurativa presents unique challenges in diagnosis and treatment, requiring a nuanced approach that balances medical intervention with patient-centered care. By understanding the range of treatment options, from topical creams to surgical procedures, and considering the latest research and expert insights, individuals affected by this condition can work towards finding relief and improving their quality of life. The future of HS management looks promising, with emerging therapies and a deeper understanding of the condition offering hope for more effective and sustainable treatments.
What are the first signs of hidradenitis suppurativa on the face?
+The first signs of facial hidradenitis suppurativa can include painful, inflamed bumps or nodules, often mistaken for acne or other skin conditions. These lesions can occur on the face, typically in areas with apocrine glands, and may be accompanied by itching, burning, or a foul odor.
Can hidradenitis suppurativa on the face be cured?
+While there is no cure for hidradenitis suppurativa, various treatments can effectively manage symptoms, reduce the frequency of flare-ups, and prevent long-term damage. Early diagnosis and a comprehensive treatment plan tailored to the individual’s needs can significantly improve the prognosis.
How does lifestyle impact hidradenitis suppurativa on the face?
+Lifestyle factors, including diet, exercise, smoking, and stress levels, can influence the severity and frequency of hidradenitis suppurativa symptoms. Maintaining a healthy weight, avoiding tight clothing, quitting smoking, and practicing stress management techniques may help reduce flare-ups and improve overall well-being.