Wound Dehiscence And Evisceration
The phenomenon of wound dehiscence and evisceration is a serious and potentially life-threatening complication that can occur after surgical procedures. Wound dehiscence refers to the partial or complete separation of previously closed surgical incisions, while evisceration is the protrusion of internal organs through the open wound. These conditions not only pose significant challenges for healthcare providers but also contribute to increased morbidity, mortality, and healthcare costs.
Understanding Wound Dehiscence
Wound dehiscence is often categorized based on its severity, ranging from minor separation of the wound edges to complete disruption of the wound, potentially leading to evisceration. The pathophysiology behind wound dehiscence is multifactorial, involving issues related to the patient’s overall health, the surgical technique employed, and post-operative care. Factors such as malnutrition, diabetes, smoking, and the use of certain medications (e.g., steroids) can impair wound healing, making dehiscence more likely.
Furthermore, surgical factors including inadequate closure technique, excessive tension on the wound edges, and infection can also contribute to the development of wound dehiscence. Understanding these risk factors is crucial for the prevention and management of wound complications.
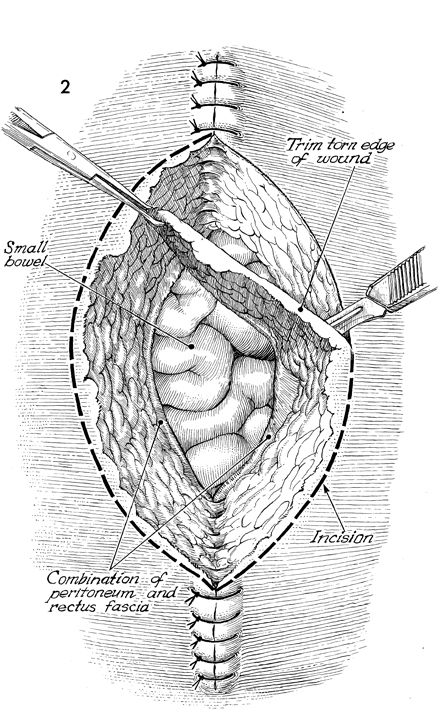
The Complexity of Evisceration
Evisceration, a more severe form of wound dehiscence, involves the protrusion of internal organs (such as the intestines) through the abdominal wall. This condition requires immediate medical attention, as it can lead to significant morbidity and mortality due to infection, organ damage, and loss of domain. The management of evisceration involves prompt surgical intervention to return the organs to their correct anatomical position and secure the wound, often requiring a multidisciplinary approach involving surgeons, intensivists, and other healthcare professionals.
Prevention Strategies
Preventing wound dehiscence and evisceration begins pre-operatively with the optimization of the patient’s health status. This includes improving nutritional status, controlling diabetes, and encouraging smoking cessation. Intra-operatively, meticulous surgical technique, ensuring a tension-free closure, and the use of appropriate suturing materials are critical. Post-operatively, monitoring for signs of wound complications, maintaining a sterile environment, and early mobilization are key strategies to reduce the risk of these complications.
Management and Treatment
The management of wound dehiscence and evisceration involves a stepwise approach, starting with stabilization of the patient, followed by surgical debridement and cleaning of the wound, and finally, closure of the wound. In some cases, temporary closure devices or wound vacuum-assisted closure may be employed to facilitate healing. Nutritional support and the management of underlying conditions are also vital components of the treatment plan.
Future Directions and Research
Research into wound dehiscence and evisceration continues to evolve, with advancements in surgical techniques, wound dressing materials, and the application of negative pressure wound therapy offering promising avenues for reducing the incidence of these complications. Moreover, the integration of biomaterials and tissue engineering into wound management holds potential for enhancing wound healing and preventing dehiscence.
Practical Application Guide
For healthcare professionals, a practical approach to preventing and managing wound dehiscence and evisceration includes:
- Pre-operative Optimization: Encourage lifestyle modifications and optimize chronic conditions.
- Intra-operative Techniques: Employ meticulous surgical technique, ensuring a tension-free wound closure.
- Post-operative Monitoring: Regularly inspect the wound for signs of complications and maintain a clean environment.
- Early Intervention: Promptly address any signs of wound dehiscence to prevent progression to evisceration.
Step-by-Step Approach to Managing Wound Dehiscence
- Assess the patient's overall condition and stabilize as necessary.
- Perform surgical debridement and cleaning of the wound.
- Consider temporary closure methods or negative pressure wound therapy.
- Provide nutritional support and manage underlying conditions.
- Plan for definitive wound closure when the patient's condition permits.
FAQ Section
What are the primary causes of wound dehiscence?
+The primary causes of wound dehiscence are multifactorial, including patient-related factors (such as malnutrition and diabetes), surgical technique issues (like inadequate closure), and post-operative complications (including infection).
How is evisceration managed?
+Evisceration requires immediate surgical intervention to return the protruded organs to their correct position and secure the wound. This often involves a multidisciplinary approach and may include temporary closure methods until definitive repair can be safely performed.
What role does nutrition play in preventing wound complications?
+Nutrition plays a critical role in wound healing. Adequate nutritional status, particularly with regards to protein, vitamins (such as Vitamin C), and minerals (like zinc), is essential for optimal wound healing and can help prevent complications like dehiscence and evisceration.
In conclusion, wound dehiscence and evisceration are serious post-operative complications that require prompt attention and a comprehensive management plan. By understanding the risk factors, preventive measures, and treatment options, healthcare professionals can work towards minimizing the incidence and impact of these conditions, ultimately improving patient outcomes and reducing healthcare costs. As research continues to evolve, the integration of innovative techniques and materials into clinical practice holds promise for further enhancing wound care and management.

