Subgingival Dental Calculus

The formation of subgingival dental calculus, also known as tartar, is a complex process that involves the accumulation of mineralized plaque below the gum line. This type of dental calculus is particularly problematic because it can lead to the development of periodontal disease, a condition characterized by inflammation and infection of the gums and bone that support the teeth.
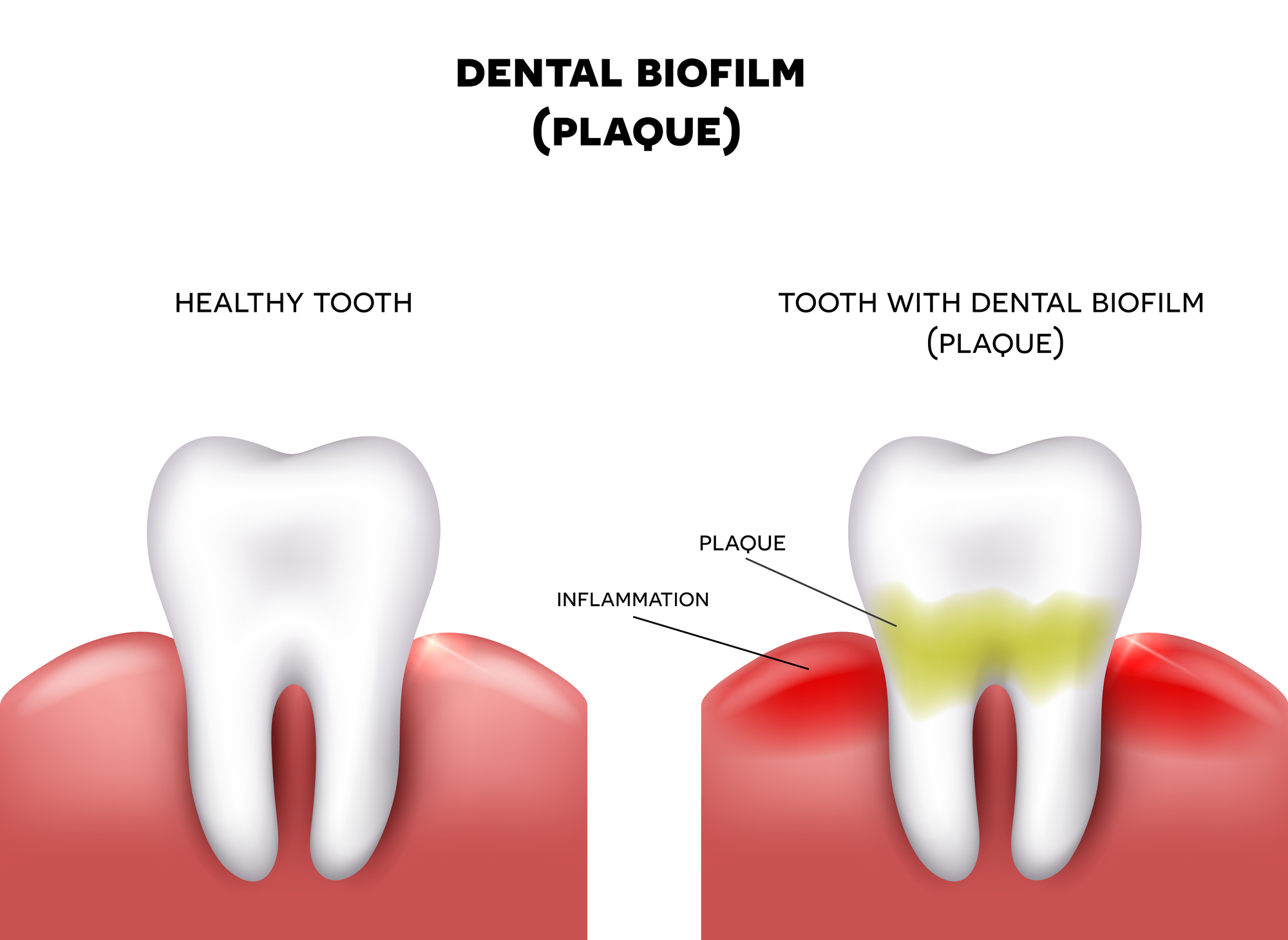
Research has shown that subgingival dental calculus is composed of a variety of microorganisms, including bacteria, archaea, and fungi. These microorganisms work together to form a biofilm, which is a community of microorganisms that adhere to a surface and are embedded in a protective matrix. The biofilm provides a safe haven for the microorganisms to grow and multiply, and it also protects them from the host’s immune system.
One of the key factors that contributes to the formation of subgingival dental calculus is the presence of gingivitis, a condition characterized by inflammation of the gums. Gingivitis can cause the gums to become swollen and bleed easily, which can lead to the accumulation of plaque and bacteria below the gum line. If left untreated, gingivitis can progress to periodontitis, a more serious condition that can cause the destruction of the bone and tissue that support the teeth.
The process of subgingival dental calculus formation is influenced by a variety of factors, including the type and amount of bacteria present, the flow of saliva and crevicular fluid, and the patient’s overall health status. For example, patients with diabetes or other systemic diseases may be more susceptible to the formation of subgingival dental calculus due to their compromised immune system.
Types of Subgingival Dental Calculus
There are several types of subgingival dental calculus, each with its own unique characteristics. Some of the most common types include:
- Supragingival calculus: This type of calculus forms above the gum line and is visible to the naked eye. It is often yellow or brown in color and can be removed with a dental scaler.
- Subgingival calculus: This type of calculus forms below the gum line and is not visible to the naked eye. It is often more difficult to remove than supragingival calculus and may require the use of specialized instruments.
- Calculaire: This type of calculus is a combination of supragingival and subgingival calculus. It forms both above and below the gum line and can be challenging to remove.
It's essential to note that subgingival dental calculus is a significant concern in the field of periodontics. The accumulation of calculus below the gum line can lead to the development of periodontal pockets, which can provide a haven for bacteria to grow and multiply. This can ultimately lead to the destruction of the bone and tissue that support the teeth, resulting in tooth loss.
Clinical Detection and Diagnosis
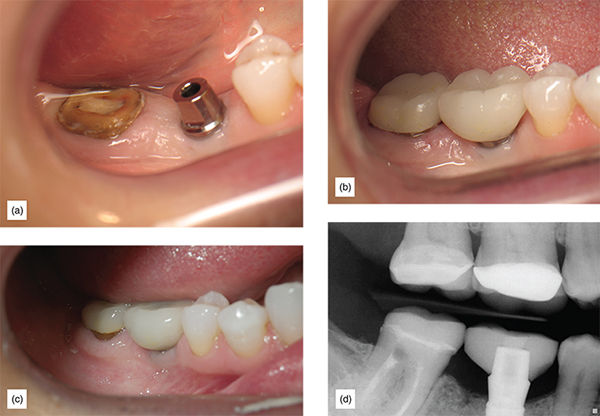
The detection and diagnosis of subgingival dental calculus typically involve a combination of visual examination, probing, and radiographic evaluation. The dentist or hygienist will use a periodontal probe to measure the depth of the pocket and assess the presence of calculus. They may also use radiographs (x-rays) to evaluate the extent of the calculus and the degree of bone loss.
In some cases, the dentist or hygienist may use a device called a periodontal chart to record the depth of the pockets and the presence of calculus. This information can be used to track the progression of the disease and the effectiveness of treatment.
Detection and Diagnosis Steps:
- Visual examination: The dentist or hygienist will visually examine the teeth and gums to look for signs of calculus and periodontal disease.
- Probing: The dentist or hygienist will use a periodontal probe to measure the depth of the pocket and assess the presence of calculus.
- Radiographic evaluation: The dentist or hygienist may use radiographs (x-rays) to evaluate the extent of the calculus and the degree of bone loss.
- Periodontal charting: The dentist or hygienist may use a periodontal chart to record the depth of the pockets and the presence of calculus.
Treatment and Prevention
The treatment of subgingival dental calculus typically involves a combination of scaling, root planing, and antimicrobial therapy. The goal of treatment is to remove the calculus and bacteria that are contributing to the disease, and to prevent further accumulation.
Scaling and root planing are procedures that involve the use of specialized instruments to remove the calculus and smooth the surface of the root. This can help to reduce the risk of further calculus accumulation and promote healing.
Antimicrobial therapy may be used in conjunction with scaling and root planing to help reduce the bacterial load and prevent further infection. This may involve the use of antibiotics or antimicrobial mouthwashes.
Prevention is also an essential aspect of managing subgingival dental calculus. This can involve regular brushing and flossing, as well as regular dental check-ups and cleanings. The use of an antimicrobial mouthwash may also be recommended to help reduce the risk of calculus accumulation.
Benefits and Drawbacks of Treatment Options:
| Option | Benefits | Drawbacks |
|---|---|---|
| Scaling and root planing | Effective in removing calculus and reducing bacterial load | May cause discomfort or sensitivity |
| Antimicrobial therapy | Helps to reduce bacterial load and prevent further infection | May have side effects or interact with other medications |
| Regular brushing and flossing | Helps to prevent calculus accumulation and promote oral health | May not be effective in removing existing calculus |

Conclusion
Subgingival dental calculus is a significant concern in the field of periodontics. The accumulation of calculus below the gum line can lead to the development of periodontal pockets, which can provide a haven for bacteria to grow and multiply. This can ultimately lead to the destruction of the bone and tissue that support the teeth, resulting in tooth loss.
The detection and diagnosis of subgingival dental calculus typically involve a combination of visual examination, probing, and radiographic evaluation. Treatment may involve scaling, root planing, and antimicrobial therapy, and prevention is also an essential aspect of managing the disease.
By understanding the causes and consequences of subgingival dental calculus, individuals can take steps to prevent its formation and promote oral health.
What is subgingival dental calculus?
+Subgingival dental calculus is a type of dental calculus that forms below the gum line. It is composed of mineralized plaque and can lead to the development of periodontal disease.
How is subgingival dental calculus detected and diagnosed?
+The detection and diagnosis of subgingival dental calculus typically involve a combination of visual examination, probing, and radiographic evaluation.
What are the treatment options for subgingival dental calculus?
+Treatment may involve scaling, root planing, and antimicrobial therapy. Prevention is also an essential aspect of managing the disease.