Peripheral Neuropathy Guide: Glutenfree Solutions
Peripheral neuropathy, a condition characterized by damage to the peripheral nerves, can manifest in a multitude of symptoms, including pain, numbness, and tingling in the hands and feet. The potential causes of peripheral neuropathy are diverse, ranging from diabetes and vitamin deficiencies to autoimmune diseases and genetic disorders. Among these, the role of gluten, a protein found in wheat, barley, and rye, has garnered significant attention in recent years. For individuals suffering from peripheral neuropathy, adopting a gluten-free diet may offer a pathway to alleviating symptoms and improving quality of life.
Understanding Peripheral Neuropathy
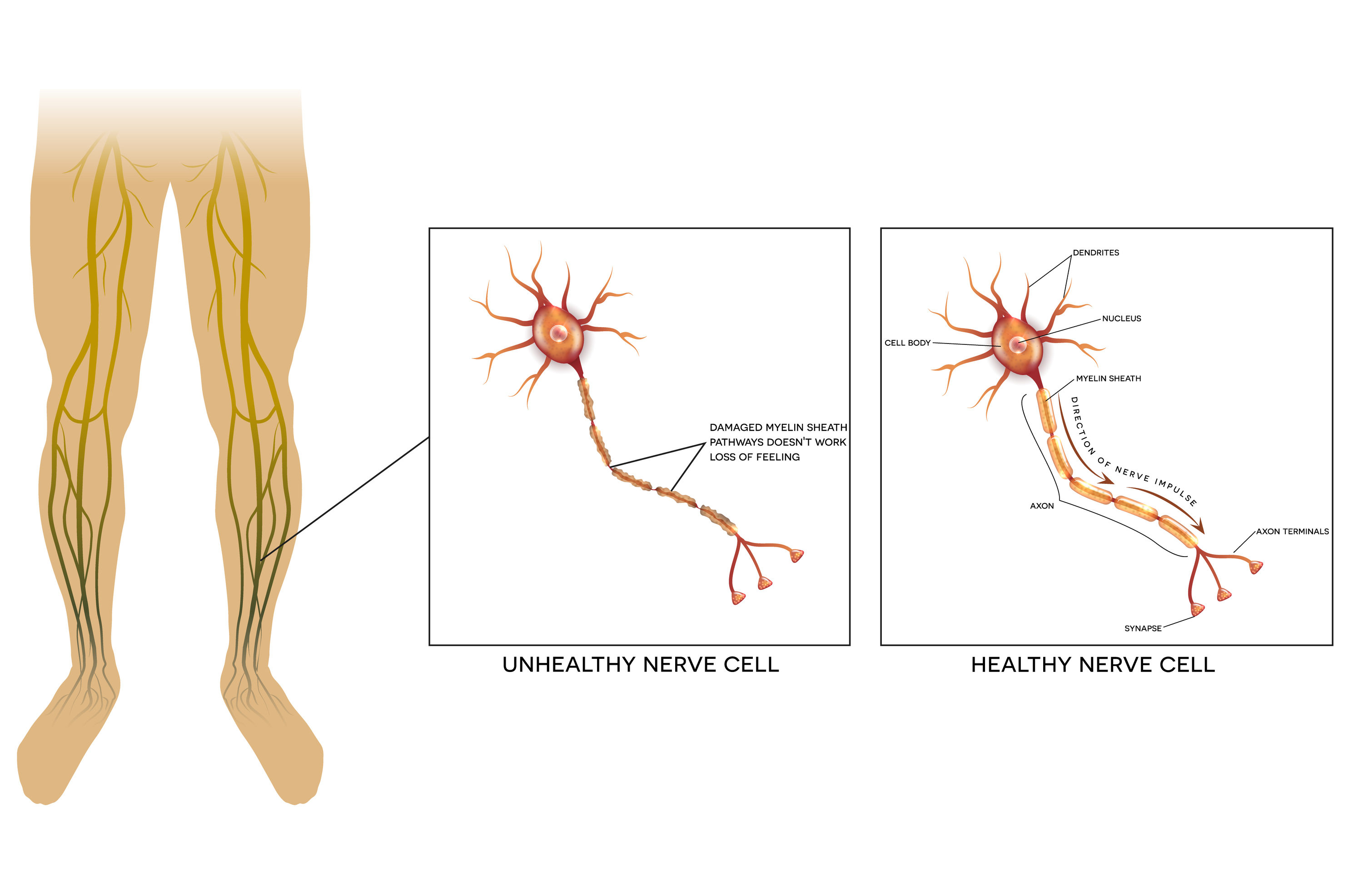
Peripheral neuropathy is not a single disease but rather a term that describes a range of disorders resulting from damage to the peripheral nervous system. This system, comprising nerves that branch out from the brain and spinal cord, is crucial for controlling voluntary actions, such as walking and talking, as well as involuntary functions, like digestion and heart rate. The symptoms of peripheral neuropathy can vary widely depending on the nerves affected. Common symptoms include:
- Pain: Sharp, stabbing, or burning pain, particularly in the feet and hands
- Numbness or Tingling: Loss of sensation or abnormal sensations like pins and needles
- Weakness: Muscle weakness or wasting, especially if motor nerves are affected
- Coordination and Balance Problems: Difficulty walking or keeping balance due to nerve damage
The Gluten Connection
Gluten, a protein found in certain grains, can trigger an autoimmune response in some individuals, leading to conditions like celiac disease and non-celiac gluten sensitivity (NCGS). There is growing evidence to suggest that gluten can also play a role in the development or exacerbation of peripheral neuropathy, particularly in those with underlying gluten-related disorders. The exact mechanisms by which gluten might contribute to peripheral neuropathy are still under investigation, but potential factors include:
- Autoimmune Response: In conditions like celiac disease, the immune system mistakenly attacks the small intestine when gluten is present. Similar autoimmune reactions could potentially target peripheral nerves, leading to neuropathy.
- Malabsorption: Damage to the small intestine from gluten can lead to the malabsorption of essential nutrients, including vitamins crucial for nerve health, such as B12.
- Inflammation: Gluten exposure can trigger inflammation in the body, which may damage peripheral nerves over time.
Implementing a Gluten-Free Diet
For individuals with peripheral neuropathy who also have celiac disease, NCGS, or those who simply wish to explore dietary interventions, adopting a strict gluten-free diet can be a significant step. Here are some key considerations and steps for transitioning to a gluten-free lifestyle:
Step 1: Consult a Healthcare Professional
Before making any significant dietary changes, it’s essential to consult with a healthcare provider. They can help determine if a gluten-free diet is appropriate and ensure that the transition is managed in a way that maintains nutritional balance.
Step 2: Identify Gluten Sources
Gluten is commonly found in wheat, barley, and rye. Less obvious sources include: - Processed foods with wheat derivatives - Some types of beer - Certain medications and supplements - Cross-contaminated foods (e.g., oats processed in facilities that also handle wheat)
Step 3: Plan Gluten-Free Meals
Focus on whole, naturally gluten-free foods like: - Fresh fruits and vegetables - Lean proteins (meat, fish, poultry, beans, and lentils) - Gluten-free grains (rice, quinoa, corn, and certified gluten-free oats) - Nuts and seeds - Healthy fats (avocado, olive oil)
Step 4: Read Labels Carefully
When shopping for packaged foods, look for the “gluten-free” label or certification from a reputable organization. Be aware that even if a product is naturally gluten-free, it may still be contaminated if processed in a facility that handles gluten-containing grains.
Step 5: Monitor Progress and Adjust
Keep a food diary to track diet changes and any corresponding shifts in neuropathy symptoms. Regular consultations with a healthcare provider can help assess the effectiveness of the gluten-free diet and guide further adjustments as needed.
Additional Dietary Considerations for Neuropathy Management
While a gluten-free diet may help alleviate symptoms for some, it’s also crucial to address overall nutritional needs. Certain nutrients, such as:
- Vitamin B12: Essential for nerve health and the synthesis of myelin, the fatty substance that surrounds and protects nerve fibers.
- Vitamin E: Acts as an antioxidant, protecting nerves from damage caused by free radicals.
- Omega-3 Fatty Acids: Help reduce inflammation and support nerve health.
- Magnesium and Potassium: Important for nerve function and signal transmission.
Ensuring adequate intake of these nutrients through diet or supplements, under the guidance of a healthcare provider, can be beneficial in managing peripheral neuropathy.
Natural Therapies and Lifestyle Changes

Beyond dietary adjustments, several natural therapies and lifestyle changes may complement treatment and enhance quality of life for individuals with peripheral neuropathy. These include:
- Physical Therapy: Customized exercises can help improve mobility, strength, and balance.
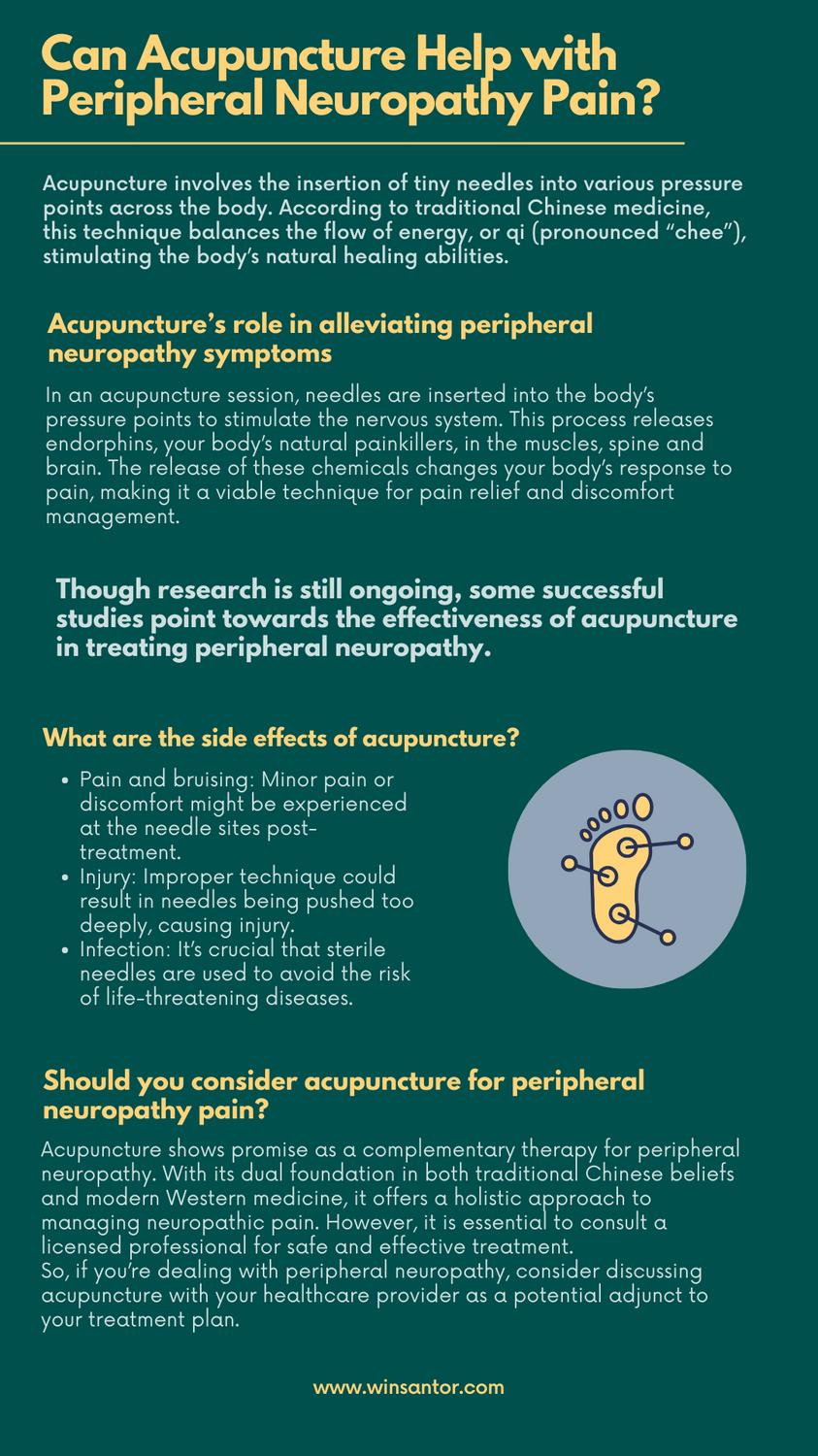
- Acupuncture: This traditional Chinese medicine technique involves inserting thin needles into specific points on the body and may help alleviate pain and improve nerve function.
- Mind-Body Therapies: Practices like meditation and yoga can reduce stress, improve mood, and increase overall sense of well-being.
- Regular Exercise: Encourages blood flow, which is vital for nerve health, and can help manage underlying conditions like diabetes.
Conclusion
Peripheral neuropathy is a complex condition that requires a multifaceted approach to management. For some individuals, adopting a gluten-free diet may be a critical component of their treatment plan, especially if they have an underlying gluten-related disorder. However, it’s also important to consider the broader nutritional and lifestyle factors that influence nerve health. By working closely with healthcare providers and exploring various dietary and therapeutic strategies, individuals with peripheral neuropathy can take proactive steps towards reducing their symptoms and improving their quality of life.
Can a gluten-free diet cure peripheral neuropathy?
+A gluten-free diet may help alleviate symptoms of peripheral neuropathy in individuals with gluten-related disorders but is not a cure for the condition. The effectiveness of a gluten-free diet can vary widely among individuals and should be implemented under the guidance of a healthcare provider.
How long does it take to notice improvements in neuropathy symptoms after going gluten-free?
+The time it takes to notice improvements in neuropathy symptoms after adopting a gluten-free diet can vary significantly among individuals. Some may experience noticeable relief within a few weeks, while for others, it may take several months. Consistency with the diet and patience are key, along with regular assessments by a healthcare provider to adjust the treatment plan as necessary.
Are there any risks or side effects of going gluten-free for peripheral neuropathy?
+While a gluten-free diet is generally considered safe, improperly planned diets can lead to nutritional deficiencies, particularly in fiber, iron, calcium, vitamin B12, and folate. It’s crucial to work with a healthcare provider or a registered dietitian to ensure that the gluten-free diet is well-balanced and meets all nutritional needs.

