Peripheral Neuropathy Gluten
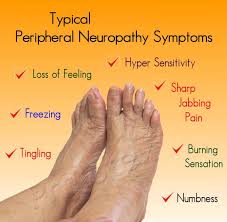
Peripheral neuropathy, a condition characterized by damage to the peripheral nerves, can manifest in various ways, including pain, numbness, and weakness in the affected areas. While the causes of peripheral neuropathy are diverse, ranging from diabetes and traumatic injuries to infections and exposure to toxins, there’s a significant interest in the potential link between peripheral neuropathy and gluten, particularly in the context of celiac disease and non-celiac gluten sensitivity (NCGS).
Gluten, a protein found in wheat, barley, and rye, has been implicated in several autoimmune and inflammatory conditions. For individuals with celiac disease, an autoimmune disorder where the ingestion of gluten leads to damage in the small intestine, the connection to peripheral neuropathy is well-documented. Studies have shown that patients with celiac disease are at a higher risk of developing peripheral neuropathy, with symptoms that can precede the gastrointestinal manifestations of the disease.
The pathophysiology behind gluten-induced peripheral neuropathy in celiac disease involves both immune-mediated damage and nutritional deficiencies. The immune response triggered by gluten can lead to the production of antibodies that may cross-react with components of the peripheral nerves, causing direct damage. Additionally, the malabsorption associated with celiac disease can result in deficiencies of essential nutrients, such as vitamin B12, vitamin E, and copper, which are crucial for the health and function of the nervous system. These deficiencies can further contribute to the development of peripheral neuropathy.
Beyond celiac disease, the role of gluten in non-celiac gluten sensitivity (NCGS) and its potential to cause peripheral neuropathy is less clear. NCGS is characterized by symptoms that resemble those of celiac disease but without the same level of immune system activation and intestinal damage. Some patients with NCGS may experience neurological symptoms, including peripheral neuropathy, but the evidence linking NCGS directly to peripheral neuropathy is largely anecdotal and requires further research to fully understand the relationship.
Diagnosis and Treatment
Diagnosing peripheral neuropathy related to gluten involves a combination of clinical assessment, laboratory tests, and sometimes nerve conduction studies or biopsy. For individuals with celiac disease, adopting a strict gluten-free diet is the primary treatment, which can lead to significant improvement or even resolution of neuropathic symptoms. However, the response to a gluten-free diet can vary, and some patients may require additional treatments to manage their neuropathy, such as vitamin supplements or medications to control pain.
In the case of NCGS, while some patients report improvement in neurological symptoms, including those of peripheral neuropathy, after removing gluten from their diet, the benefit is not universally observed, and the decision to try a gluten-free diet should be made under the guidance of a healthcare provider.
Gluten-Free Diet and Peripheral Neuropathy
A gluten-free diet is the cornerstone of managing gluten-related disorders, including celiac disease. For individuals with peripheral neuropathy attributed to gluten, the diet involves avoiding foods that contain gluten and focusing on gluten-free alternatives. This requires careful reading of food labels, awareness of hidden sources of gluten in processed foods, and potentially seeking the advice of a dietitian to ensure a balanced and nutritious diet.
Future Directions
The relationship between gluten and peripheral neuropathy, especially in the context of NCGS, is an area of ongoing research. Further studies are needed to elucidate the mechanisms by which gluten may contribute to neuropathic symptoms in individuals without celiac disease and to establish clear guidelines for the diagnosis and management of gluten-related peripheral neuropathy.
In conclusion, while the link between gluten and peripheral neuropathy is established in the context of celiac disease, the situation is more nuanced for non-celiac gluten sensitivity. A comprehensive approach to diagnosis and treatment, considering both the potential for gluten-induced damage and the importance of nutritional deficiencies, is crucial for managing peripheral neuropathy in patients with gluten-related disorders.
FAQ Section
Can peripheral neuropathy be caused by gluten sensitivity?
+While the direct link between non-celiac gluten sensitivity (NCGS) and peripheral neuropathy is not as well-established as it is for celiac disease, some individuals with NCGS may experience neuropathic symptoms. However, more research is needed to fully understand this relationship.
How is gluten-related peripheral neuropathy diagnosed?
+Diagnosis involves a combination of clinical evaluation, laboratory tests to rule out other causes of neuropathy, and sometimes specific tests for celiac disease or gluten sensitivity. A trial of a gluten-free diet may also be recommended to assess symptom improvement.
Can a gluten-free diet improve peripheral neuropathy symptoms?
+For individuals with celiac disease, a strict gluten-free diet is crucial and can lead to improvement or resolution of neuropathic symptoms. For those with non-celiac gluten sensitivity, the response to a gluten-free diet can vary, and the decision to try this approach should be made under medical guidance.
Conclusion
The intersection of gluten and peripheral neuropathy underscores the complex interplay between diet, immune response, and neurological health. As research continues to unravel the mechanisms behind gluten-induced neuropathy, adopting a personalized approach to diet and treatment, under the guidance of healthcare professionals, remains essential for managing symptoms and improving quality of life for affected individuals.

