Osgood Schlatter Disease Causes Revealed
Osgood Schlatter disease, a condition characterized by knee pain in adolescents, has puzzled parents and healthcare professionals alike for decades. The affliction, named after the American orthopedic surgeons Robert Bayley Osgood and Carl B. Schlatter, who first described it in the early 20th century, affects the tibial tubercle, a bony prominence at the top of the shinbone. This article delves into the causes, symptoms, and treatment options of Osgood Schlatter disease, providing a comprehensive understanding of this complex condition.
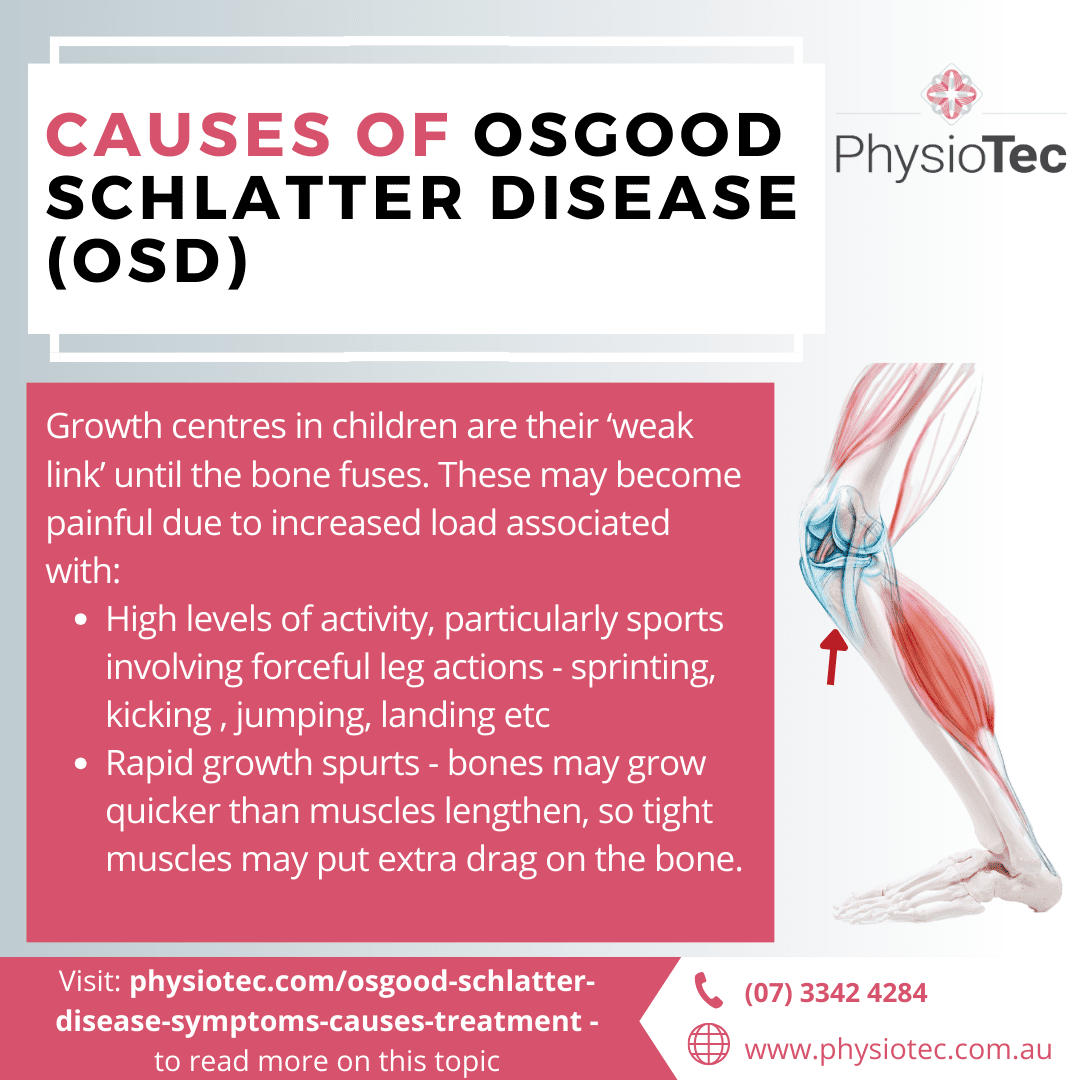
Understanding the Anatomy
To grasp the causes of Osgood Schlatter disease, it’s crucial to understand the anatomy involved. The tibial tubercle is the site where the patellar tendon attaches to the tibia. This tendon plays a vital role in straightening the knee. During adolescence, the bones, muscles, and tendons undergo rapid growth, which can lead to inflammation and irritation at the tibial tubercle. This inflammation is the hallmark of Osgood Schlatter disease.
Growth Spurts and Overuse
Two primary factors contribute to the development of Osgood Schlatter disease: growth spurts and overuse. During puberty, bones grow faster than muscles and tendons, leading to tightness and increased stress on the tendons, particularly the patellar tendon. This stress can cause inflammation at the tibial tubercle. Furthermore, adolescents who participate in sports that involve frequent running, jumping, or quick changes of direction are more prone to overuse injuries, which can exacerbate the condition.
Symptoms and Diagnosis
The primary symptom of Osgood Schlatter disease is pain below the knee, which typically worsens with activity and improves with rest. A bony bump may also be visible at the tibial tubercle. Diagnosis is usually based on a physical examination and medical history, as imaging tests like X-rays are not always necessary. However, in some cases, an X-ray may be used to rule out other conditions, such as a fracture.
Treatment and Management
While Osgood Schlatter disease can be painful and bothersome, it is a self-limiting condition, meaning it will resolve on its own once growth is complete. Treatment focuses on managing symptoms and reducing inflammation. Common management strategies include:
- Rest and Activity Modification: Avoiding or reducing activities that aggravate the condition is crucial.
- Ice and Compression: Applying ice to the area and using a compressive bandage can help reduce pain and swelling.
- Physical Therapy: Stretching and strengthening exercises can help alleviate symptoms and improve knee function.
- Pain Relief: Over-the-counter pain medications may be recommended to manage discomfort.
Prevention
Preventing Osgood Schlatter disease is challenging, given its association with growth and development. However, adolescents can reduce their risk by:
- Gradually Increasing Activity Levels: Sudden increases in physical activity should be avoided.
- Warming Up and Cooling Down: Proper warm-up and cool-down routines can help prevent overuse injuries.
- Strengthening Core and Leg Muscles: Stronger muscles can better absorb the stresses of activity.
What are the common symptoms of Osgood Schlatter disease?
+The common symptoms include pain below the knee, which worsens with activity and improves with rest. A visible bony bump may also be present at the tibial tubercle.
How is Osgood Schlatter disease diagnosed?
+Diagnosis is usually based on a physical examination and medical history. Imaging tests like X-rays may be used in some cases to rule out other conditions.
Can Osgood Schlatter disease be prevented?
+While it cannot be completely prevented, the risk can be reduced by gradually increasing activity levels, properly warming up and cooling down, and strengthening core and leg muscles.
Conclusion
Osgood Schlatter disease is a common condition affecting adolescents, particularly those involved in sports. Understanding its causes, recognizing its symptoms, and adopting appropriate management strategies are key to alleviating its impact. While it is a self-limiting condition that resolves with time, taking preventive measures can help reduce the risk and severity of symptoms. As with any health condition, consulting a healthcare professional for personalized advice and treatment is essential for the best outcomes.

