12+ Corrected Csf Wbc Secrets For Improved Patient Care

Cerebrospinal fluid (CSF) analysis is a critical diagnostic tool in neurology, providing valuable insights into various neurological conditions. One crucial aspect of CSF analysis is the examination of white blood cell (WBC) count, which can indicate the presence of inflammation, infection, or other abnormalities within the central nervous system (CNS). Understanding the intricacies of CSF WBC interpretation is essential for healthcare professionals to deliver accurate diagnoses and effective patient care. This article delves into the secrets of corrected CSF WBC counts, exploring their significance, interpretation, and implications for improved patient outcomes.
Introduction to CSF and WBC
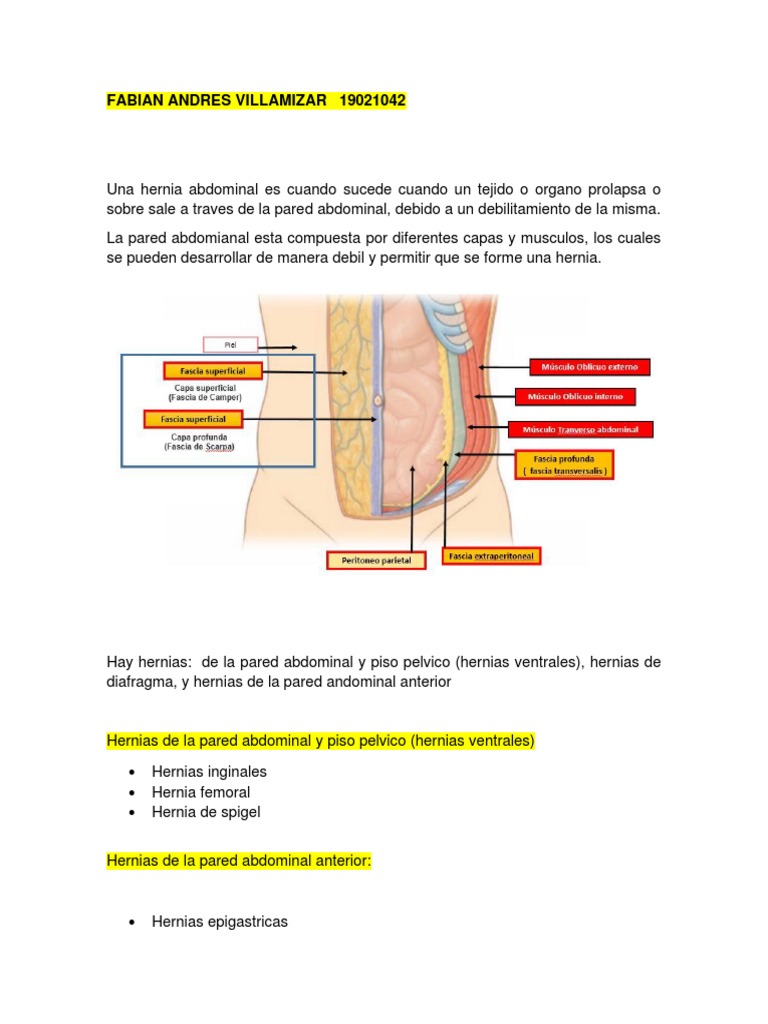
Cerebrospinal fluid circulates through the brain and spinal cord, acting as a cushion and providing immunological protection. The presence of white blood cells (WBCs) in the CSF can signal an immune response, which may be due to infection, inflammation, or other pathological processes. The corrected WBC count in CSF is a calculated value that adjusts for the presence of red blood cells (RBCs), which can contaminate the sample during a traumatic lumbar puncture. This correction is vital for accurate interpretation, as the presence of RBCs can falsely elevate the apparent WBC count.
The Importance of Corrected WBC Count
The corrected WBC count is calculated using the formula: (CSF WBC count x 100) / (CSF RBC count + 100). This calculation helps to differentiate between a traumatic tap and true CNS inflammation or infection. For instance, a high uncorrected WBC count due to RBC contamination might suggest an inflammatory process, whereas the corrected count could reveal a more benign condition, thereby avoiding unnecessary diagnostic tests and treatments.
Interpretation of CSF WBC Count
Interpreting CSF WBC counts requires a comprehensive understanding of clinical context, including patient symptoms, medical history, and results of other diagnostic tests.
Normal Range: A normal CSF WBC count is typically considered to be fewer than 5 cells/μL, with the majority being lymphocytes or monocytes. The presence of neutrophils or elevated numbers of lymphocytes can indicate an acute infection or inflammatory process.
Elevated WBC Count: An elevated corrected WBC count suggests an immune response within the CNS. This could be due to various conditions, including bacterial meningitis, viral encephalitis, multiple sclerosis, or cerebrovascular accidents. The differential count of WBCs (e.g., neutrophil predominance in bacterial infections vs. lymphocytic predominance in viral infections) can provide crucial clues to the underlying cause.
Clinical Correlation: It’s essential to correlate the CSF findings with clinical presentation. For example, a patient with symptoms of meningitis (fever, headache, stiff neck) and an elevated CSF WBC count is more likely to have a CNS infection than a patient with similar CSF findings but no such symptoms.
The Role of Technology in CSF Analysis
Advancements in laboratory technology have significantly improved the accuracy and efficiency of CSF analysis. Automated cell counters and flow cytometry can provide rapid and precise WBC counts, reducing the reliance on manual microscopy and minimizing human error. Moreover, molecular diagnostics, such as PCR (polymerase chain reaction), can detect specific pathogens in the CSF, aiding in the diagnosis of infections.
Impact on Patient Care
The accurate interpretation of corrected CSF WBC counts has a direct impact on patient care. It guides the selection of appropriate antimicrobial therapy, determines the need for further diagnostic tests, and informs prognosis. For example, a patient with bacterial meningitis requires immediate antibiotic therapy, whereas a patient with viral meningitis may require supportive care only. Misinterpretation of CSF results can lead to delayed or inappropriate treatment, potentially worsening outcomes.
Complications and Limitations
While CSF analysis is a powerful diagnostic tool, it is not without limitations. A traumatic lumbar puncture can lead to contamination, and the presence of blood in the CSF can complicate the interpretation of WBC counts. Additionally, certain conditions, such as tuberculous meningitis, may present withnormal or only slightly elevated WBC counts in the early stages, highlighting the need for repeated sampling and correlation with clinical findings.
Advanced Diagnostic Techniques
The integration of advanced diagnostic techniques, including next-generation sequencing and mass spectrometry, into CSF analysis holds promise for improving diagnostic accuracy and speed. These technologies can identify a broad range of pathogens, including those that are difficult to culture or are present in low quantities, thereby facilitating targeted therapy and reducing the risk of empirical treatment failures.
Conclusion
In conclusion, the corrected CSF WBC count is a vital component of neurological diagnosis, offering insights into the presence and nature of CNS inflammation or infection. Healthcare professionals must understand the nuances of CSF analysis, including the calculation and interpretation of corrected WBC counts, to provide accurate diagnoses and effective care. By combining clinical expertise with advances in laboratory technology and maintaining awareness of the limitations and potential complications of CSF analysis, healthcare providers can optimize patient outcomes in a wide range of neurological conditions.
Practical Application Guide
For healthcare professionals seeking to improve their interpretation of CSF WBC counts, the following steps are recommended: 1. Ensure Proper Sample Handling: Correct handling and processing of CSF samples are crucial to avoid contamination and ensure accurate results. 2. Calculate Corrected WBC Count: Always calculate the corrected WBC count to adjust for RBC contamination, especially in cases of traumatic lumbar puncture. 3. Correlate with Clinical Findings: Interpret CSF results in the context of the patient’s clinical presentation, medical history, and other diagnostic findings. 4. Stay Updated with Diagnostic Advances: Familiarize yourself with new technologies and techniques in CSF analysis to improve diagnostic accuracy and speed.
Future Trends Projection
The future of CSF analysis holds much promise, with ongoing research into novel biomarkers, advanced diagnostic technologies, and personalized medicine approaches. As our understanding of the CNS and its immune responses evolves, so too will the role of CSF analysis in neurological diagnosis and treatment. The integration of AI and machine learning into laboratory diagnostics may further enhance the accuracy and efficiency of CSF WBC count interpretation, contributing to better patient care and outcomes.
What is the significance of a corrected WBC count in CSF analysis?
+The corrected WBC count in CSF analysis adjusts for the presence of red blood cells, which can contaminate the sample during a traumatic lumbar puncture, thereby providing a more accurate indication of CNS inflammation or infection.
How does the interpretation of CSF WBC count impact patient care?
+Accurate interpretation of CSF WBC counts guides the selection of appropriate treatments, determines the need for further diagnostic tests, and informs prognosis, thereby directly influencing patient outcomes.
What are the limitations of CSF analysis in diagnosing neurological conditions?
+CSF analysis has limitations, including potential contamination during sample collection, and certain conditions may present with normal or slightly elevated WBC counts in early stages, requiring repeated sampling and correlation with clinical findings.